Overactive bladder is a common condition in which there is a sudden intense urge to urinate. At times, it may be followed by an involuntary loss of urine (urge incontinence). Patients typically feel a bladder muscle contraction which gives a warning of only a few seconds to a minute to reach a restroom. The condition is also associated with frequent urination, and urination at night. This condition occurs in both men and women and increases with age. Although a cause is not always identified, onset of symptoms may occur after menopause, prostate problems, infections, neurologic injury such as stroke or multiple sclerosis, diabetes, prior surgery, radiation, and dietary issues.
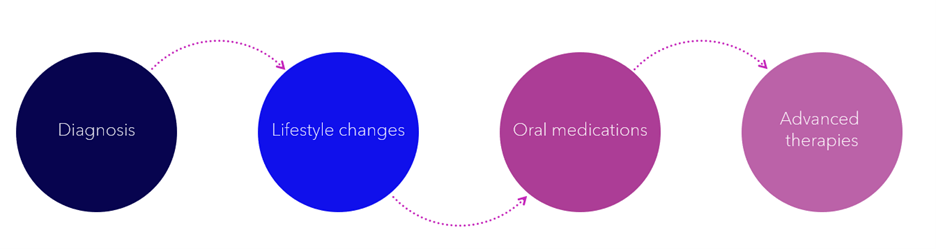
First line treatment involves addressing any identifiable cause of symptoms, behavioral modification and diet change. There are a number of FDA approved medications for the treatment of this common condition. If symptoms persist, further workup with post void residual measurement, cystoscopy and complex urodynamics may be necessary. We offer a range of advanced treatment options for the difficult to treat cases.
Percutaneous tibial nerve stimulation (PTNS) is a series of weekly treatments, similar to the concepts of acupuncture, that are performed in the office. Botox® injection in the bladder is another treatment option that may help improve symptoms for the next 3-6 months. InterStim™ sacral neuromodulation is an effective surgical treatment that is reserved for the most difficult cases.
Treatment Options
There are many ways to manage bladder control problems. Remember, if conservative treatments don’t deliver the results you need, you have more options.
Lifestyle Changes1
Conservative treatments can help some people but may not work very well (or at all) for others. All of these are relatively simple behavioral changes that you may already be doing.
- Diet and exercise: Changes may include decreasing your caffeine intake and getting more exercise.
- Bladder retraining: Also called biofeedback, this involves delaying going to the bathroom and sticking to a strict schedule.
- Pelvic floor strengthening: This can be accomplished through Kegel exercises, which involve repeatedly contracting and relaxing the muscles of the pelvic floor.
Oral Medications
When lifestyle changes fail to deliver the results you want, oral medications are the next step. These medications can help control symptoms but may cause other issues.
You have to remember to take these medications every day. Some side effects can be unpleasant, such as dry mouth, blurry vision, constipation, and hypertension.2 Other side effects are more serious. In fact, data suggests that one class of drugs for OAB (anticholinergics) may increase risk of dementia in elderly people.3 Even more important, these medications don’t always work. In one survey, 72% of people said they stopped taking their medication after just six months.4
Advanced Therapies
If conservative treatments don’t deliver the results you want, you have more options.
Medtronic Bladder Control Therapy Delivered by The InterStim™ System
- Try it during an evaluation
- Proven long-term relief5
Implanting an InterStim™ system has risks similar to any surgical procedure, including swelling, bruising, bleeding, and infection. Talk with your doctor about ways to minimize these risks. Complications can occur with the evaluation, including movement of the wire, technical problems with the device, and some temporary pain. Your doctor or nurse will provide you with the information regarding how to operate the test device and inform you of other precautions related to the evaluation and activity restrictions.
Information on this site should not be used as a substitute for talking with your doctor. Always talk with your doctor about diagnosis and treatment information.
*Medtronic Bladder Control Therapies do not treat obstructive urinary retention.
1. American Urological Association. Diagnosis and treatment of non-neurogenic overactive bladder (OAB) in adults: an AUA/SUFU guideline. www.auanet.org/guidelines/overactive-bladder-(oab)-guideline. Accessed August 5, 2020.
2. Haab F, Castro‐Diaz D. (2005), Persistence with antimuscarinic therapy in patients with overactive bladder. Int J Clin Prac, 59: 931-937.
3. Gray S, Anderson M, Dublin S et al. Cumulative use of strong anticholinergics and incident dementia. JAMA Intern Med. 2015;175(3):401-407.
4. Yeaw J, Benner J, Walt JG et al. Comparing adherence and persistence across 6 chronic medication classes. J Manag Care Pharm. 2009:15(9): 724-736.
5. Siegel S, Noblett K, Mangel J, et al. Five year follow-up results of a prospective, multicenter study in overactive bladder subjects treated with sacral neuromodulation. 2018; 199(1), 229-236.
For more in depth information on Overactive Bladder (OAB), please refer to this Urology Care Foundation™ link: Overactive Bladder (OAB): Symptoms, Diagnosis & Treatment



